Treatment of large varicose leg veins has advanced significantly over the past 15 years. Previously, most large varicose veins were treated through an in-hospital procedure known as “vein stripping” but, the postoperative recovery can be painful and prolonged. Today, virtually all large varicose veins are treated through office-based procedures. Endovenous Laser Therapy or EVLT, also called “endovenous laser ablation” is a minimally invasive procedure that permanently seals the vein closed, preventing blood from pooling.
When EVLT is combined with a microphlebectomy (which removes smaller varicosities), the results are significantly enhanced. EVLT is a highly effective and safe treatment for varicose veins. The post- procedure recovery is usually uneventful, with patients experiencing minimal discomfort, bruising or swelling. Usually, you can return to normal activities within a few days.
When EVLT received FDA approval in 2002, DR. SADIQ HUSSAIN, MD was the first vascular surgeon in the Port Huron area to learn the procedure. He has treated over 900 patients over the last 16 years and delivered exceptional results. In medicine, there is no replacement for experience.
Small varicose veins are sometimes best eliminated using a procedure called microphlebectomy. During microphlebectomy, surgeon makes a tiny incision in the skin and the varicose vein is removed. The procedure is done with local anesthesia and no stitches are needed. Patients are only required to wear compression stockings for a few days after the procedure. Typically, there is minimal discomfort, and excellent results are immediate.
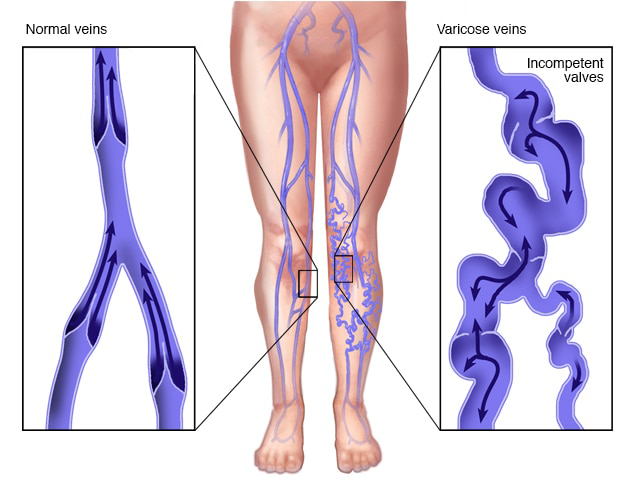
Varicose veins are gnarled, enlarged veins. Any vein may become varicose, but the veins most commonly affected are those in your legs and feet. That's because standing and walking upright increases the pressure in the veins of your lower body.
For many people, varicose veins and spider veins — a common, mild variation of varicose veins — are simply a cosmetic concern. For other people, varicose veins can cause aching pain and discomfort. Sometimes varicose veins lead to more-serious problems.
Varicose veins may also signal a higher risk of other circulatory problems. Treatment may involve self-care measures or procedures by your doctor to close or remove veins.
When EVLT is combined with a microphlebectomy (which removes smaller varicosities), the results are significantly enhanced. EVLT is a highly effective and safe treatment for varicose veins. The post- procedure recovery is usually uneventful, with patients experiencing minimal discomfort, bruising or swelling. Usually, you can return to normal activities within a few days.
Varicose veins may not cause any pain. Signs you may have with varicose veins include:
When painful signs and symptoms occur, they may include:
Self-care — such as exercise, elevating your legs or wearing compression stockings — can help you ease the pain of varicose veins and may prevent them from getting worse. But if you're concerned about how your veins look and feel and self-care measures haven't stopped your condition from getting worse, see your doctor.
Arteries carry blood from your heart to the rest of your tissues. Veins return blood from the rest of your body to your heart, so the blood can be recirculated. To return blood to your heart, the veins in your legs must work against gravity.
Muscle contractions in your lower legs act as pumps, and elastic vein walls help blood return to your heart. Tiny valves in your veins open as blood flows toward your heart then close to stop blood from flowing backward.
Causes of varicose veins can include:
These factors increase your risk of developing varicose veins:
Age The risk of varicose veins increases with age. Aging causes wear and tear on the valves in your veins that help regulate blood flow. Eventually, that wear causes the valves to allow some blood to flow back into your veins where it collects instead of flowing up to your heart.
Sex Women are more likely to develop the condition. Hormonal changes during pregnancy, premenstruation or menopause may be a factor because female hormones tend to relax vein walls. Taking hormone replacement therapy or birth control pills may increase your risk of varicose veins.
Family history If other family members had varicose veins, there's a greater chance you will too.
Obesity Being overweight puts added pressure on your veins.
Standing or sitting for long periods of time Your blood doesn't flow as well if you're in the same position for long periods.
Complications of varicose veins, although rare, can include:
UlcersExtremely painful ulcers may form on the skin near varicose veins, particularly near the ankles. Ulcers are caused by long-term fluid buildup in these tissues, caused by increased pressure of blood within affected veins.
A discolored spot on the skin usually begins before an ulcer forms. See your doctor immediately if you suspect you've developed an ulcer.
Blood clots Occasionally, veins deep within the legs become enlarged. In such cases, the affected leg may swell considerably. Any sudden leg swelling warrants urgent medical attention because it may indicate a blood clot — a condition known medically as thrombophlebitis.
Bleeding Occasionally, veins very close to the skin may burst. This usually causes only minor bleeding. But, any bleeding warrants medical attention because there's a high risk it can happen again.
There's no way to completely prevent varicose veins. But improving your circulation and muscle tone can reduce your risk of developing varicose veins or getting additional ones. The same measures you can take to treat the discomfort from varicose veins at home can help prevent varicose veins, including: